Krystal Rampalli, DFC research assistant, discusses myths and realities of food choice research.
Perhaps one of the more remarkable effects of globalization is that one can find virtually anything anywhere. Never has this been more obvious than with food choices and food systems. For example, there are probably more Washington apples at roadside produce stalls in rural Jharkhand, India than the local harvest. Rather than traditional snacks, you will find Oreo cookies and Snickers candy bars lining the aisles of supermarkets in urban Lusaka, Zambia. With thousands of choices at one’s fingertips, making decisions about what to get, for who, where, why, and how to prepare and eat can become rather complicated. On the surface, this might sound like a typical “First World Problem,” but nowadays, these choices are not just possible in high-income countries. The issues that drive these food choices transcend borders, but little is known about how these processes occur in low and middle-income countries (LMICs).
The goal of the Drivers of Food Choice Competitive Grants Program is to fund projects that examine the drivers of food choice among the poor, particularly in the 41 LMICs that make up 90% of the global burden of undernutrition. The projects examine the interconnected biological, psychological, economic, social, cultural and political factors that affect the individual and community-level decision-making process of what is ultimately consumed, and the impacts such decisions have on individual and community health (1). Before we can go into the nuances of food choice research, we must dispel some commonly cited myths associated with food choice as they pertain to LMICs around the world.
Myth #1: The primary nutrition issues in LMICs are related to hunger or undernutrition.
Reality: Most LMICs are in the midst of what Popkin and colleagues at the University of North Carolina describe as a nutrition transition – a shift in dietary patterns from traditional, often nutrient-dense foods to more processed, energy-dense convenience foods. Drastic changes in food consumption, along with reduced physical activity, are a byproduct of increased urbanization and modernization. In most high-income countries, this same nutrition transition took place around five decades prior, particularly as more women opted to work outside the household. At the population level in both high-income countries and LMICs, there has been a noticeable increase in body weight and the incidence of lifestyle-related conditions, such as type II diabetes and cardiovascular disease (2). In many LMICs, a double burden of malnutrition exists in which there is simultaneous hunger and undernutrition as well as obesity and diet-related non-communicable diseases. There is also the increased problem of hidden hunger, a type of undernutrition characterized not by a lack of energy, but rather, by micronutrient deficiencies that stem from consumption of energy-dense foods that lack vitamins and minerals that are necessary to sustain one’s life (2–6).

Young women harvesting tomatoes in rural Indonesia (Photo credit: Krystal Rampalli)
Myth #2: People in LMICs do not have a choice in food – they eat what they can afford and what is available where they live.
Reality: While some areas may have limited variety, most people have a choice to make about food – and it is more complicated than one might expect. While it is generally true that urban food environments offer more diverse options than rural environments, throughout the process of making food choices there are decisions to be made, regardless of where one lives. Considerations about what to grow or raise, sell, trade, or buy, who will buy it, when to buy, where to buy food, as well as how to cook it (if it will be cooked), where to cook it, when to cook it, who will cook it. There are also decisions about serving and eating – who will be served, what, where, when, why and how, and then as the end user, what will be eaten, how much will be eaten, when, where, and why. At every level, there are tradeoffs. For example, deciding whether to cook and eat at home or eat out might be influenced by the resource of time; the time it would take to find, purchase, and consume a restaurant meal might be a fraction of the time it would take to find, purchase, prepare, and consume a homemade dish. For some people, however, the time loss incurred by cooking at home might well be worth the higher monetary cost of eating outside. For others, it may not be worth it. With an increasing number of women in LMICs working outside the home, the time potentially available for major household activities, such as cooking, is significantly reduced (7). Regardless of the reason(s), the food-choice decisions depend on a complex array of elements, beyond simply economic, including sociocultural, psychological, and environmental (8). Understanding determinants of food choice is important for shaping effective health, food, and nutrition promotion strategies and policies for the future.

One of several choices in daily outdoor markets in urban Lusaka, Zambia (Photo credit: Krystal Rampalli)
Myth #3:Focusing on food choice devalues the importance of the food environment.
Reality:Food choices are made within the backdrop of both personal and external food environments (9). Infrastructure quality, agricultural subsidies and policies, changes in retail food markets, land permanence, urbanization, shifts in livelihood opportunities, and changing gender roles are just some aspects of environments that influence food choice (1). A July 2018 article in the New York Times profiling the diabetes epidemic in Mexico illustrates this reality. In the town of San Cristóbal de las Casas, residents report purchasing Coca-Cola and other sugar-sweetened beverages over water. This was in part explained by the lack of a wastewater treatment plant in town, and that bottled drinking water is more expensive than sugar-sweetened beverages. Beyond these environmental drivers in San Cristóbal de las Casas, there are also personal drivers at play that cannot be understood by looking at only the external environment. For example, this indigenous community holds spiritual beliefs that there are healing powers in carbonated beverages, and they are widely consumed during religious ceremonies (10). This case study illustrates how both personal and external environmental factors can shape food-choice decisions in a community (9). Furthermore, individuals react to their environment(s) differently. For example, one person may respond to a marketing message more positively than another person. Some families in San Cristóbal de las Casas may be willing to spend more on water or travel farther to get water for personal, health, or other reasons. Some simply may not like the taste of sugar-sweetened beverages and refuse to purchase them. These preferences may be driven more by personal factors, such as genetics, rather than access. There is a growing body of research in the genetic aspects of consumer preference, such as why some people favor sugary food over savory food, and why some are more prone to diabetes than others (11). To devise viable policies and public health promotion strategies, individual food choices must be understood as they are situated within the context of personal and external food environments.
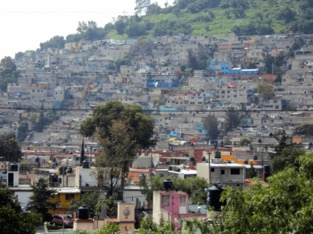
Low income housing in Mexico City, Mexico. (Photo credit: Krystal Rampalli)
Myth #4: If you make healthy food available to people, they will consume it.
Reality: Sometimes. Acquiring and consuming healthy food can be taxing, financially and otherwise, for many in both high-income countries and LMICs. Despite financial barriers addressed in some contexts, cultural and religious beliefs might still hinder consumption of nutritious foods. For example, followers of the Jain religion in India avoid all animal-sourced products, which can potentially lead to various protein and micronutrient deficiencies if alternate foods are not equivalent in nutritive value (12). For another example, an accepted method to promote healthy eating among lower-income families is through social safety net cash-transfer programs in both high-income countries and LMICs. These interventions seek to increase food security and demand for food, and ultimately, improve nutrition outcomes by increasing a household’s purchasing power. Some have specific conditions for recipients, such as keeping their children in school, while others are unconditional, with blanket transfers of money or issuance of redeemable vouchers at specified intervals. These programs have been tried in several countries across the globe with variable effectiveness; some studies have found that despite having more purchasing power presumably to spend on healthier food options, some family members were still undernourished. Other impact evaluations of food-assistance programs have shown that they can to alleviate the damaging effects that poverty has on health. Sometimes concerns are expressed that cash-transfer monies may have been spent on non-nutritious food, alcohol, or tobacco, or that goods were purchased and later sold, or that there are personal and sociocultural norms and perceptions around certain foods that prohibit or reduce consumption (13–15). Even if these concerns hold true, cash-transfer programs are one of several examples of how people will still prioritize and exercise their right to choose, even if a so-called better option is feasible.

A bustling city market in Nashik, Maharashtra, India (Photo credit: Krystal Rampalli)
References
- Drivers of Food Choice Competitive Grants Program [Internet]. 2018 [cited 2018 Jun 30]. Available from: https://driversoffoodchoice.org
- Muthayya S, Rah JH, Sugimoto JD, Roos FF, Kraemer K, Black RE. The Global Hidden Hunger Indices and Maps: An Advocacy Tool for Action. PLoS One. 2013;8:1–12.
- Popkin BM. The Nutrition Transition and Obesity in the Developing World. J Nutr. 2001;131:871–3.
- Popkin BM. The nutrition transition in low-income countries : An emerging crisis. Nutr Rev. 1994;52:285–98.
- Popkin BM. The nutrition transition and its health implications in lower-income countries. Public Health Nutr. 1998;1:5–21.
- Gödecke T, Stein AJ, Qaim M. The global burden of chronic and hidden hunger: Trends and determinants. Glob Food Sec [Internet]. Elsevier B.V.; 2018;17:21–9. Available from: https://doi.org/10.1016/j.gfs.2018.03.004
- Johnston D, Stevano S, Malapit HJ, Hull E, Kadiyala S. Review: Time Use as an Explanation for the Agri-Nutrition Disconnect: Evidence from Rural Areas in Low and Middle-Income Countries. Food Policy [Internet]. Elsevier; 2018;76:8–18. Available from: https://doi.org/10.1016/j.foodpol.2017.12.011
- Hardcastle S, Thøgersen-Ntoumani C, Chatzisarantis N. Food Choice and Nutrition: A Social Psychological Perspective. Nutrients [Internet]. 2015;7:8712–5. Available from: http://www.mdpi.com/2072-6643/7/10/5424
- Agriculture N and HAFEWG (ANH-F. Concepts and methods for food environment research in low and middle-income countries. London, UK; 2017.
- Lopez O, Jacobs A. In Mexican Town, Soda Is Everywhere. So Is Diabetes. New York Times [Internet]. New York, NY; 2018;A6. Available from: https://www.nytimes.com/2018/07/14/world/americas/mexico-coca-cola-diabetes.html
- Larson N, Story M. A review of environmental influences on food choices. Ann Behav Med. 2009;38.
- Shah AH, Battalwar R. A study on the nutritional status of Jain women. Int J Food Sci Nutr [Internet]. 2017;2:91–4. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=med3&AN=7659698%5Cnhttp://sfx.bib-bvb.de/sfx_ubm?sid=OVID:medline&id=pmid:7659698&id=doi:&issn=0921-9668&isbn=&volume=47&issue=3&spage=201&pages=201-9&date=1995&title=Plant+Foods+for+Hum
- Leroy JL, Ruel M, Verhofstadt E. The impact of conditional cash transfer programmes on child nutrition: a review of evidence using a programme theory framework. J Dev Eff [Internet]. 2009;1:103–29. Available from: http://www.tandfonline.com/doi/full/10.1080/19439340902924043
- Ruel MT, Alderman H. Nutrition-sensitive interventions and programmes: How can they help to accelerate progress in improving maternal and child nutrition? Lancet. Elsevier Ltd; 2013;382:536–51.
- Jensen ML, Frongillo EA, Leroy JL, Blake CE. Participating in a Food-Assisted Maternal and Child Nutrition and Health Program in Rural Guatemala Alters Household Dietary Choices. J Nutr [Internet]. 2016;146:1593–600. Available from: http://jn.nutrition.org/cgi/doi/10.3945/jn.116.232157
